What is the Role of the Pharmacy Benefits Manager?
Pharmacy Benefits Manager, or PBMs, are third-party businesses that contract with government programs and employer-sponsored health plans to manage pharmacy benefits. PBMs create and manage prescription formularies, negotiate rebates and contracts with manufacturers, and supervise the processing and payment of pharmacy benefit claims.
Recently, some healthcare experts and advocates have expressed concern that the services provided by PBMs do not provide sufficient positive value to justify their high costs and impact on the overall cost of health care.
PBMs have a considerable behind-the-scenes impact on deciding total drug costs for insurers, influencing patients’ access to prescriptions, and dictating how much pharmacies are compensated. The increased scrutiny has been directed at PBMs about their participation in escalating prescription drug costs and expenditures.
What impact do PBMs have on the cost of prescription drugs?
PBMs work in the center of the prescription drug distribution chain. As a result, they:
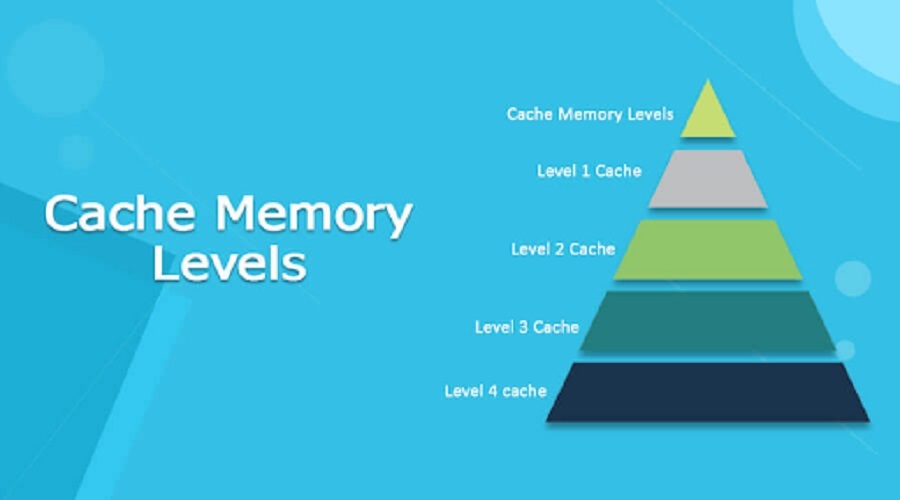
- Create and manage lists, or formularies, of covered prescriptions on behalf of health insurers, which determine which drugs patients use and their out-of-pocket expenses.
- Utilizing their purchasing power to negotiate rebates and discounts with pharmaceutical manufacturers
- contract directly with individual pharmacies to compensate beneficiaries for medications dispensed.
The federal Centers for Medicare and Medicaid Services discovered that the capacity of PBMs to negotiate larger rebates from manufacturers had helped reduce prescription prices and slowed the growth of drug expenditures over the past three years. However, PBMs may also incentivize the promotion of expensive pharmaceuticals over more cost-effective ones. Because rebates are frequently determined as a percentage of the manufacturer’s list price, pharmacy benefit managers (PBMs) receive a more significant rebate for expensive pharmaceuticals than those that may give more excellent value at a lower cost. Consequently, those with high-deductible plans or copayments based on a drug’s list price may suffer higher out-of-pocket expenses.
What controversy surrounds the Rebates PBMs receive from Drug Manufacturers?
Drug manufacturers allege that rising rebates paid to pharmacy benefit managers (PBMs) force them to hike list prices. Recent research indicates that rebates from manufacturers to pharmacy benefit managers (PBMs) grew from $39.7 billion in 2012 to $89.5 billion in 2016, mainly offsetting list price hikes. Four PBMs argue that they have passed on a more significant portion of rebates to insurers.
There is considerable controversy about whether PBMs should be allowed to retain the rebates they earn from drug makers, which are often not made public. Some feel that PBMs should be required to “pass through” all or a significant percentage of these cost reductions to health insurers and other payers. If PBMs were forced to do this, insurers could use the savings to lower premiums and cost-sharing payments for individuals. According to a recent survey, the proportion of rebates that PBMs passed on to insurers and payers climbed from 78% in 2012 to 91% in 2016. However, many small insurers and businesses report not receiving this portion of savings.
A further dispute involves a PBM practice known as “spread pricing,” Health insurers and employers reimburse PBMs for generic pharmaceuticals at a higher price than the PBMs pay pharmacies. The PBMs then retain the remainder. Again, a lack of openness makes this possible: health plans are not privy to the payment schedules that PBMs generate for pharmacies.
What have regulatory improvements been recommended for PBMs?
Policymakers have suggested three major modifications for PBMS regulation. Demand greater openness regarding refunds. Federal and state officials require further data on rebates received by PBMs to acquire a more comprehensive view of pharmaceutical spending and potential reform areas.
Prohibit spread pricing. Policymakers might outlaw the practice to ensure that payers and businesses are not overpaying PBMs for prescription medications. A more limited plan would require PBMs to amend their pricing schedules with pharmacies to reflect generic medicine price rises.
Demand that PBMs transmit rebates to payers or patients. PBMs could be compelled to pass on 90 percent of their rebate savings to payers to preserve some of their incentive to negotiate price reductions with medication manufacturers. Alternately, PBMs may be mandated to pass rebates on to patients. The federal government has suggested mandating that PBMs associated with Medicare Part D plans to pass on at least one-third of the rebates and price concessions they obtain to patients.
Some analysts believe that PBMs should realign their business strategy away from getting rebates and enhancing pharmaceutical expenditures’ value. For instance, health insurers and pharmacy benefit managers (PBMs) should do more to assist physicians in prescribing the most cost-effective pharmaceuticals on their patients’ formularies. And PBMs might base formulary decisions and price negotiations on a drug’s health benefits and total cost of patient care.
Criticism of the PBM Business
As implied by the company’s nature, PBMs are frequently the subject of lawsuits and government investigations. PBMs have not consistently revealed rebates, discounts, itemized billing statements, and the proportion of savings passed on to insurers as third-party negotiators with opaque business methods.
State legislatures have been pressing for increased openness and disclosure rules to govern these corporations effectively. In addition, there has been pressure to require PBMs to behave in the best interest of insurers and insurance plans, comparable to the legal obligation of financial advisors to act in the best interest of their customers. This suggests that the PBM sector may be subject to regulations that could harm future profitability.
Ensuring Accessibility, Safety, and Cost-Savings
PBMs eliminate waste from the system and ensure patient safety. When a patient fills a prescription, we work in the background to analyze the patient’s prescription history, confirm the exact dosage, screen for any drug interactions, and guarantee that the medication is inexpensive.
And compassionate care is available 24/7 with a simple phone call.
PBMs also bring value by examining the thousands of medications that have been authorized for usage. An independent panel of physicians and pharmacists examines the pharmaceuticals in-depth and compiles a formulary — a list of medications with the best clinical outcomes for all illnesses.
By delivering more innovative solutions to patients and clients, pharmacy benefit managers (PBMs) provide better care and lower costs with every prescription. For more information visit https://spectrumpsp.com.